How to Write Patient Notes Clearly and Quickly
Writing a good patient note is like telling a short, clear story about a person's health. The best way to learn how to write patient notes is to be very careful and use a simple plan, like the SOAP plan. This helps any doctor or nurse read the note and know right away what is happening with the patient and what to do next.
Why Clear Patient Notes Matter More Than You Think

Think of a patient's chart as their health diary. Every note you write is a new page in that diary. These notes are not just busy work. They are the main tool that helps the whole medical team work together.
When notes are simple and easy to read, they help stop bad mistakes. They also help doctors, nurses, and other helpers share ideas easily. When everyone understands, the patient is much safer.
The Shift to Digital Records
Most hospitals and clinics now use computers for patient notes. This is called an electronic health record (EHR). In 2021, most doctors—almost 9 out of 10—were using an EHR system. Using computers makes it fast and easy to share the patient's health story.
Imagine a patient needs to see a new doctor. A well-written note gives that new doctor the whole story at once. This helps them make better choices and keep the patient safe. New tools are helping, too. Many doctors now use special software to write notes just by talking. You can learn more about this in our guide to voice recognition software for healthcare.
A patient note is a message for the team first and a legal paper second. If another doctor can't understand your note, it has failed at its most important job.
Learning the benefits of medical voice charting shows how important clear notes are for keeping patients safe and helping doctors work better. No matter how you write them, a good note is always:
- Easy to understand: Anyone on the team should be able to read it and know what to do.
- True: It must be exactly right about the patient and their care.
- Complete: It should have all the important parts without extra words that make it confusing.
Using the SOAP Method to Organize Your Notes
Think of the SOAP method as a simple recipe for your patient notes. It's a way to train your brain to put all the patient's information into a neat, clear story. Once you get used to it, you'll be able to write your notes much faster.
The word SOAP helps you remember the four parts of the note:
- S is for Subjective (what the patient says)
- O is for Objective (what you see and find)
- A is for Assessment (what you think is wrong)
- P is for Plan (what you will do to help)
When you use this recipe, any other person on the team can quickly find the part they need. It makes a story that goes from what the patient feels, to what you find, to what you think is wrong, and finally, to what you will do.
The Four Simple Parts of a SOAP Note
Each part of a SOAP note has a special job. You start with Subjective, which is the patient's story. This is where you write down what they tell you. You write about their feelings and what is bothering them, using their own words if you can.
Next is the Objective part. This is for facts you can see or measure. It’s like being a detective and finding clues. Here, you write down things like temperature, heart rate, and what you find when you check the patient. You don't guess here, you just write the facts.
This picture shows how the parts work together.
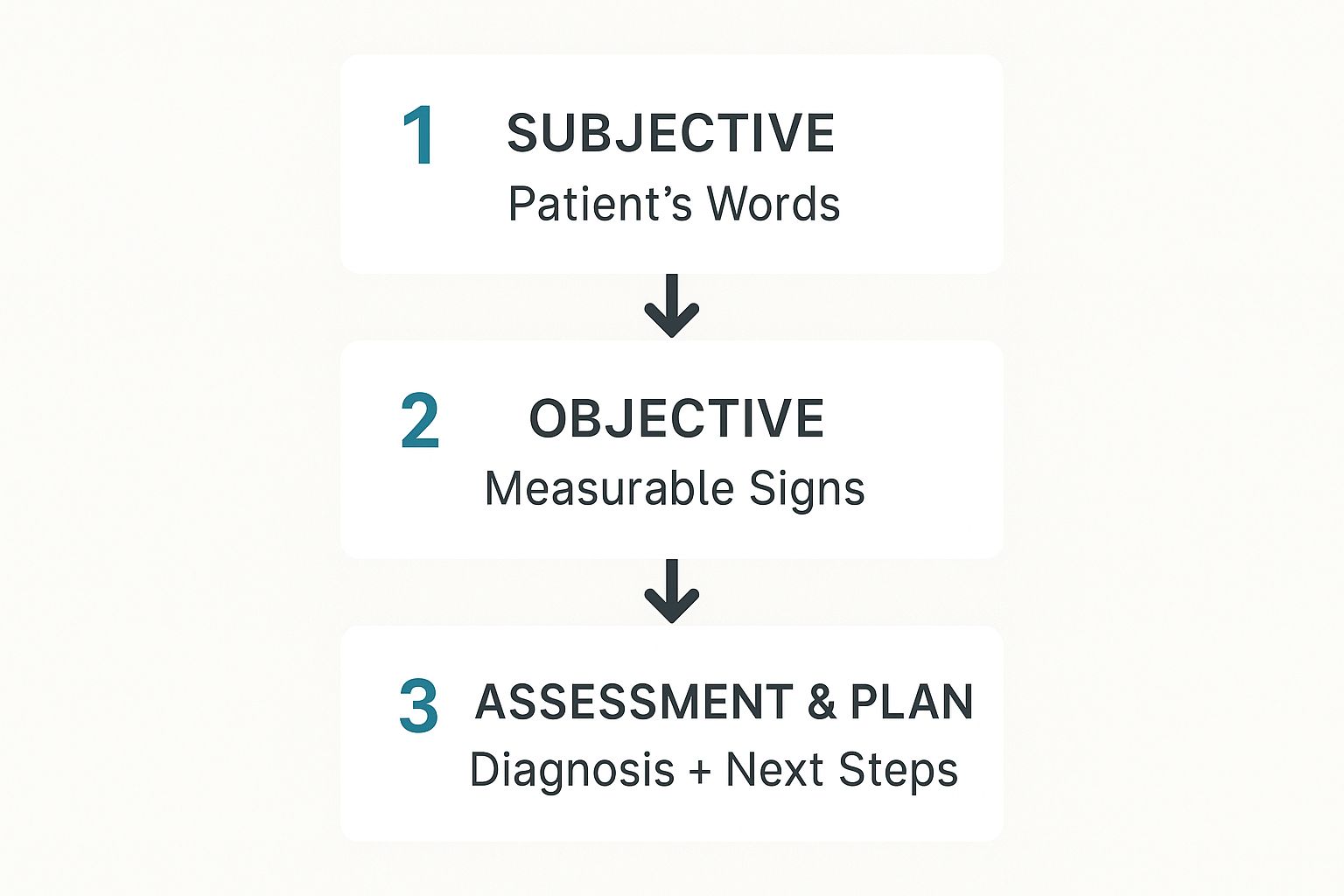
As you can see, you start with the patient's words and add the facts you find. This simple path helps you figure out what is wrong and what to do next.
Putting It All Together in Your Note
After you have the story and the clues, you are ready for the Assessment and Plan. The Assessment is what you, the expert, think is going on. You put the clues from the Subjective and Objective parts together to name the problem.
Finally, the Plan tells everyone what will happen next. It's your action list. What will you do for the patient? This could be ordering tests, giving medicine, sending them to another doctor, or asking them to come back. A good plan is very clear so no one gets confused.
Learning the SOAP format helps you think in an organized way. It turns a jumble of information into a clear story that leads to action.
To make it even simpler, here is a chart that shows how each part works with a real example.
A Simple Guide to SOAP Note Sections
| Section (SOAP) | What to Write | Real-World Example |
|---|---|---|
| Subjective | What the patient tells you. Their story. | "My head has been hurting for three days. It feels like a dull pain behind my eyes." |
| Objective | Facts you can see, measure, or test. | Temperature is 100.5°F. Blood pressure is 120/80. Face is not sore when I touch it. |
| Assessment | What you think the problem is. Your diagnosis. | Sinus infection. A headache from stress is not likely because of the fever. |
| Plan | What you are going to do to help. | 1. Suggest medicine for pain (acetaminophen). 2. Tell them to rest and drink lots of water. 3. Call in 2 days if not feeling better. |
If you use this plan every time, learning how to write patient notes will become easy. Your notes will be clear, complete, and very helpful for the patient's care.
Capturing the Patient's Story and Your Findings
Great patient notes start with one simple thing: listening. Before you write anything, you need to hear the patient's story. This is the Subjective part of your note. It's all about what the patient tells you—their feelings, worries, and what hurts.
Think of yourself as a reporter. Your job is to write down what you hear, without changing it. If a patient says, “My tummy has hurt for two days,” you write exactly that. Using their own words makes the note real and keeps all the little details.
This part is very important because it gives you the first clues. It also shows the patient you are really listening to them. Don't add your own ideas here. For now, it's just their story.
The Subjective Note: What to Include
When you are learning how to write patient notes, the subjective part is where you write the main problem and its story. A little checklist in your head can help you remember what to ask.
- Main Problem: What is the one big reason they came to see you?
- When It Started: Did it start today? Yesterday? A week ago?
- What It Feels Like: Ask them to use words to describe the feeling. Is it sharp? Dull? Aching?
- Where It Is: Can they point to the spot that hurts?
- What Makes It Better or Worse: Does resting help? Does moving hurt?
Writing all this down can take a lot of time, especially with patients who have a long story. Many doctors now use tools that listen and type for them. You can see how this works by looking at different kinds of speech to text software.
The Objective Note: What to Include
After you hear the patient's story, it’s time to be a detective. This is the Objective part of the note. It’s all about facts—things you can see, measure, and prove.
This is where you write down numbers like temperature, heart rate, and blood pressure. You also write what you find when you check the patient's body. The key here is to be very clear. "The patient has a rash" is not very helpful.
The clues you find in the Objective part help you solve the patient's health puzzle. The clearer your clues, the clearer the final picture will be.
Instead, you could write: "A red, bumpy rash is on the left arm. It is about the size of a quarter and does not turn white when I press it." This gives the next person who reads the note a perfect picture of what you saw.
Being clear and writing only facts in this part is a rule you can't break. It gives the proof for your ideas in the Assessment and Plan.
Connecting the Clues and Making a Plan
https://www.youtube.com/embed/07Z4ywfmLg8
Okay, you've listened to the patient and you've found your clues. Now for the most important part of your note: the Assessment and the Plan. This is where you show how you think like a doctor. These two parts explain what you think is wrong and what you will do about it.
What's Your Assessment?
The Assessment is not just a guess. It is your expert idea based on all the clues you have. It connects what the patient said (like "my throat hurts") with what you found (like "the tonsils are red and swollen").
Just writing down the problem, like "sore throat," is not enough. The best notes explain why you think that is the problem. It’s like showing your work in math. It helps other people on the team understand your thinking.
So, how do you write a good one?
Instead of just writing "Viral sore throat," a much better assessment would be:
"The patient’s sore throat, low fever, and lack of swollen glands all point to a virus, not a bacteria like strep."
See the difference? That small sentence shows that you thought about other problems and explains why you chose this one.
A great Assessment answers the "So what?" question. It explains what all the clues mean and gets you ready to make a great plan.
Building a Clear and Actionable Plan
Once you have your Assessment, the Plan should be easy to write. This is your to-do list for the patient. You must be very clear. Writing something like "continue care" is not helpful to anyone.
A good plan is easy to follow. Anyone on the team should be able to read it and know exactly what to do. It should list every step, like medicines, tests, what to teach the patient, and when to come back.
Here are a few tricks for making your plans super clear:
Use numbers for each step. This is so simple but makes the plan easy to read. For example:
- Start Amoxicillin 500mg, three times a day for 10 days.
- Gargle with warm salt water for throat pain.
- Follow up in 3 days if not feeling better.
Be specific. Don’t just write "tell patient to rest." What does that mean? It's better to write: "Tell patient to avoid hard activities and try to sleep 8 hours a night."
Write down what you taught the patient. A quick note like, "Told patient why it is important to finish all the medicine, even if they feel better."
This kind of detail means there is no confusion. It helps the patient remember what to do and lets other doctors or nurses continue the care easily. A great plan is the last step to a note that really helps the patient.
Practical Tips for Faster and Smarter Charting
Let's be real—writing patient notes can feel like a lot of work. But it doesn't have to be so hard. With a few smart habits, you can write notes much faster and still do a great job.
The goal is to get you back to what is most important: helping patients, not typing. These small changes can save you hours every week. This helps you feel less tired and makes you less likely to make mistakes.
Use Your EHR’s Built-In Shortcuts
Most computer health record (EHR) systems have tools to help you work faster. You just have to learn how to use them. Almost every hospital uses these systems now. You can learn more about how they became so popular in this detailed report.
Here are two of the best shortcuts to learn:
- Templates: These are like fill-in-the-blank forms for common visits, like a check-up or a visit for high blood pressure. They give you a starting point so you don't have to write the same note from scratch every time.
- Dot Phrases: These are secret codes you make up. When you type the code, a whole sentence or paragraph pops up. For example, typing ".normalexam" could fill in a whole note for a healthy check-up.
Think of dot phrases as your own secret language for notes. A few taps on the keyboard can save you from typing the same thing over and over.
Document Right After the Visit
It's easy to save all your notes for the end of the day. But waiting can make the job harder. The details of a visit are freshest in your mind right after the patient leaves the room.
If you wait for hours, you might forget small but important things the patient said. Writing the note right away makes it more true and stops a big pile of work from waiting for you at the end of the day.
Some doctors even use tools that listen to the visit to help write the note in real time. You can learn more about these tools in our guide to medical voice recognition software.
Focus Only on What’s Relevant
A big mistake people make is writing down too much. Your note should be a short, clear summary of the visit, not every single word that was said. Stick to the facts that are important for the patient's problem and your plan to fix it.
For example, if a patient is here for a twisted ankle, you don't need to write a lot about their hay fever unless it has to do with the ankle problem. Keeping your notes short and to the point makes them easier for others to read and much faster for you to write. Learning how a medical scribe helps can give you more ideas on how to make notes better.
Navigating the Tricky Parts of Patient Notes
Even with a good plan, writing patient notes can be tricky. Real life is messy, and sometimes you won't be sure what to do. Let's talk about two common problems.
I Made a Mistake in My Note—Now What?
It happens to everyone. The important part is not that you made a mistake, but how you fix it. You need to be honest. You can't just erase the mistake and hope no one sees it. That can look like you are hiding something and can get you into big trouble.
The wrong words have to stay, but you can show they are wrong. Here is the right way to fix a mistake:
- Draw one straight line through the wrong words so you can still read them.
- Write your initials and the date next to the line.
- Add the right information nearby and label it "correction" or "add-on."
Think of it like this: An honest, clear fix shows you are responsible. Hiding a mistake makes people not trust you and can ruin the whole medical record.
What Do I Do When a Patient Overshares?
You are trying to learn about their main problem, and they start telling you about family drama or their last vacation. It's good to be friendly, but your note must stick to what is important for their health.
Your note is a professional paper, not a diary of your chat. You have to be a filter. If a patient is there for knee pain but talks for ten minutes about their neighbor, your note should only have the facts about their knee.
Learning how to write patient notes well means knowing what to leave out. Stick to the facts another doctor would need to understand the problem and help the patient. If a detail doesn't help with the diagnosis, the plan, or the patient's health story, it probably doesn't belong in the note.
Ready to make charting faster and easier? WriteVoice turns your spoken words into perfectly formatted text in any app, letting you create detailed notes in a fraction of the time. Reclaim your day and focus on what matters most—your patients. Try WriteVoice for free and see how much time you can save.